+91 9310434361
Enquiry Us
Diabetes

Why Is Colorectal Surgery Needed?
Colorectal Surgery is mainly done to repair any kind of damage suffered by a patient’s anus, rectum, or colon. This damage to these parts could be the result of a medical disorder, disease of the lower intestinal passageway, injury/obstruction, as well as damaged blood vessels that require surgical procedure for repairing.
...At times, abnormal tissue mass, or scar tissue can be seen developing within the rectum, which results in blocking the natural passing of bowels. There are also other common medical diseases, such as ulcerative colitis and diverticulitis that are known to cause damage to the rectum. Removing the obstruction or treating these parts with surgical procedures is known to be the ideal treatment method for restoring normal bowel movement and overall health in the patient.
Types of Colorectal Surgeries
As mentioned earlier, colorectal surgery is an umbrella term including a number of surgical procedures that are useful for a variety of medical disorders affecting the anus, rectum, or colon. This treatment is ideal for colorectal cancer, Crohn’s disease, ulcerative colitis, certain types of diverticulitis, and other medical disorders that cause an obstruction in the lower intestine passage. Hemorrhoids, bowel incontinence, rectal prolapse, and anal fissures may also require a person to have a minor form of colorectal surgery for better treatment.
Most colorectal surgeries are aimed at repairing torn inner tissue, removing obstructions, or tightening the sphincter muscles. Certain colorectal specialist surgeons are also known to successfully treat pelvic floor disorders, such as perineal hernia and rectocele with colorectal surgery.
As mentioned earlier, colorectal surgery contains several different types of surgical procedures that are meant to treat a specific colorectal disorder.
Common Types of Colorectal Surgeries
- Resection: Resection involves cutting/removing the damaged/diseased portion of the lower intestine.
- Anastomosis: Anastomosis involves re-attaching the resection ends of the lower part of the intestines together.
- Tucks: Tucks are small surgical procedures that involve tightening the loosened/prolapsed sphincter muscles, as well as repairing anal fissures and removing hemorrhoids.
- Strictureplasty: Strictureplasty is an innovative colorectal surgical procedure that involves widening the intestine to make it shorter in length. This treatment is ideally used to treat extensive damage from Crohn’s disease.
- Ostomy: These are a collective bunch of colorectal procedures that are basically aimed at creating an opening from the intestine to outside the body for passing bowel through an alternate route. A colostomy connects the large intestine to an opening in the abdomen (stoma) which passes bowels out of the body into an attached pouch. Ileostomy requires removing the anus, rectum, and colon completely, and making the small intestine a stoma (opening in the abdomen).
When is Colorectal Surgery Needed?
Colorectal Surgery is not always the first choice of treatment in mild cases of medical disorders affecting the colorectal region. However, the doctor/physician will decide whether you will need colorectal surgery after considering various factors, such as your age, health status, underlying medical disorders, etc., as well as the extent of spread and damage by the disease.
As most often, there has to be significant changes made in your lifestyle after certain colorectal surgeries, the doctor/physician/surgeon will advise you on all the pre-surgical and post-surgical care which you will be required to take for best results.
Risks Associated with Colorectal Surgery
As is seen in any major surgery, colorectal surgical procedures are also not completely devoid of certain surgical risks, such as:
- Infection
- Swelling
- Pain
- Hemorrhage
However, the surgeon will ensure every preventive measure is taken to avoid these risks from developing.
ALAAFIYAH CARE is the leading medical tourism healthcare provider. ALAAFIYAH CRE maintains a vast network of global-standard hospitals in major destinations across the world, including India, US, UK and Dubai among others for the best treatment to patients. ALAAFIYAH CARE offers effective, fast and affordable colorectal surgeries to patients from all over the world.
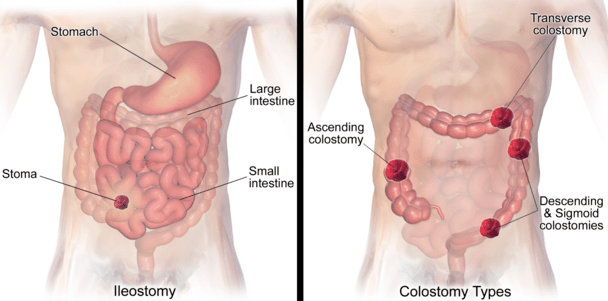
What is a Colostomy?
A Colostomy is major surgery that creates an opening (known as a “stoma”) in the colon to permit waste to exit outside the body into a pouch attached to the abdomen. Generally, in a colostomy, part of or the entire colon is removed.
A Colostomy may be permanent or temporary, depending on the medical condition that has necessitated the surgery. A temporary colostomy is to allow the colon to rest after surgery. In time, the two sections of the colon will be reconnected, and the bowels will work in the normal fashion.
...A permanent colostomy is customarily performed when the rectum or most of the colon is removed. This may be necessary due to conditions such as:
- Colon cancer
- Diverticulitis
- Crohn’s Disease
- Colon obstruction
- Birth defects
Types of Colostomies
- Ascending: This is the least common type of colostomy. A stoma is made in the first section of colon, the ascending colon, on the right abdomen. The skin is easily irritated with this kind of stoma because the stool contains digestive enzymes and is mostly liquid.
- Transverse: Two separate stomas are created in this form of colostomy. These stomas can be located in the upper abdomen, middle, or right side. One stoma is for the evacuation of stool waste, and the other stoma is to allow mucus to drain. The stool is liquid to semi-formed. This is often a temporary colostomy.
- Descending or Sigmoid: The stomas are located on the descending or sigmoid portion of the colon. The stomas are usually created on the left lower abdomen. Stool is semi-formed to fully formed. A descending or sigmoid colostomy is the most commonly performed permanent colostomy surgery. Approximately 42,000 to 65,000 ostomy surgeries are performed each year. Half of these surgeries are temporary.
Colostomy Surgery
A colostomy is performed under general anaesthetic. You will be unconscious and not feel any pain.
You may have a tube inserted through your nose into your stomach. This tube removes gas and prevents nausea and vomiting. It is possible a urinary catheter will also be used.
A colostomy can be carried out as open surgery or laparoscopically (several small surgical incisions are used to insert an instrument called a laparoscope which views and completes the operation).
Regardless of the method of surgery, the surgeon will remove the part or all of the colon that is diseased or malfunctioning. The healthy end of the colon will be brought to an abdominal opening made by incision and sewn to your abdominal skin. You may have drainage tubes in your incision.
After surgery, you go into the recovery room for monitoring until the anaesthetic has worn off. You will then be taken to your hospital room.

High Quality Ileostomy Surgery
Ileostomy surgery at low cost and high quality is now within reach through ALAAFIYAH CARE. Our nurses arrange all aspects of your treatment and will act as your patient advocate.
What is an Ileostomy?
...The ileum is the lower section of the small bowel. It connects to the large bowel. If a portion of the large bowel has to be removed due to bowel disease, ileostomy surgery is performed.
An ileostomy creates an opening in the ileum to allow waste elimination. An ileostomy can be either temporary or permanent. Medical conditions, which may cause the necessity for an ileostomy, are:
- Severe inflammatory bowel disease
- Bowel injuries
- Bowel obstruction
- Bowel cancer
- Bowel infections
Ileostomy Surgery
An ileostomy procedure is performed under general anaesthetic. An opening in the side of your abdomen will be created by the surgeon. This is called a “stoma”. Usually, the stoma is on your right lower abdomen. The surgeon will remove the portion of the bowel that is causing your medical condition.
For a traditional ileostomy, a section of the ileum is then extracted through the opening and sutured to your abdominal skin. An adhesive plastic bag is placed on the abdomen over the stoma for waste evacuation.
With a traditional ileostomy, bowel contents continuously drain into the ileostomy bag. With a continent ileostomy, there is no waste bag. Instead, an internal pouch made from intestinal tissue is created and attached to the abdominal wall. Waste contents do not continuously drain. In this case, the pouch is emptied with a narrow tube inserted into the pouch anywhere from 2 to 7 times daily.
There are risks involved with ileostomy surgery. These include general anaesthetic risks, bleeding, infection, hernia, scarring, stenosis (narrowing) of the stoma, bowel obstruction, and dehydration. Your doctor can give you complete information regarding all the risks surrounding ileostomy surgery.
Ileostomy Preparation
Preparation for an ileostomy can begin up to two weeks prior to the surgery date.
Your doctor may request you stop taking anti-coagulant medications (aspirin, Advil, anti-inflammatories) at this time. If you have a cold or flu prior to your surgery date, you need to let your doctor know as soon as possible. Surgery may have to be delayed if this is the case.
You should drink lots of water and eat a high fiber diet. Closer to your surgery, you will likely be asked to start a clear fluids only diet. No fluids or foods will be permitted after midnight the evening before your surgery.
You may be given antibiotics prior to surgery to remove bacteria from your colon. Additionally, you will be placed on a bowel-cleansing regime with laxatives or enemas a day or two before the procedure. Your bowel must be empty and clean for surgery to prevent infection. You will be in the hospital 6 to 10 days after surgery.
Pre-Surgery Arrangements
If necessary, you should arrange, in advance, for the following responsibilities before your surgery:
- Child care
- Pet care
- A house sitter, if necessary
- Payment of your financial obligations
Ileostomy Recovery
After surgery, you will be given a fluid diet until your bowel begins to function again. Once this happens, solids will be gradually permitted.
This may be within two days or may take a little longer. Before discharge from the hospital, you will be taught how to use a stoma pouch and care for your stoma.
It is important the area around the stoma be kept clean to reduce skin irritation. Stoma pouches are odor-resistant and invisible under your clothing.
Emptying the pouch when it is 1/3 full prevents bulging that may become apparent.
The number of times a pouch needs to be emptied daily varies widely.
After the first six months, you may find the necessity to empty the pouch decreases.
Pouches are replaced every 3 to 7 days. You should avoid strenuous exertions for the first three months after your surgery.
Normal everyday activities can resume 4 to 8 weeks post-surgery.
The average return to work after an ileostomy is 2 to 3 months. Using a stoma pouch may be difficult to adjust to in the beginning.
In time, you will be more at ease with the care and use of a stoma pouch.
This may take several weeks to months. Requiring ileostomy surgery and a stoma pouch can be psychologically distressing.
If you are experiencing anxieties, you should speak with your health professionals about coping strategies.
Contacting a support group may also be beneficial. Patients who undergo an ileostomy often have an improved quality of life.
